

Alcohol and Liver Disease
The pathogenesis of liver disease associated with alcohol ingestion is incompletely understood. What is known is that some patients who chronically abuse alcohol develop liver disease, primarily because the liver metabolizes the majority of ingested ethanol. Furthermore, the metabolism of ethanol is required for hepatic injury to occur, although variations in ethanol metabolism do not completely explain the variable susceptibility to alcohol-associated liver disease.
This topic review will focus on three issues related to the development of alcoholic liver disease:
Ethanol is metabolized via several pathways, each of which can contribute to toxicity. The primary hepatic pathway generates acetaldehyde and reduced nicotinamide adenine dinucleotide (NAD).
In addition, accessory inducible microsomal pathways may be responsible for the generation of toxic metabolites from several drugs, while a possible role for gastric ethanol metabolism remains controversial.
Ethanol is metabolized first in the liver to acetaldehyde; this process occurs in the hepatocyte cytosol via a reaction catalyzed by the enzyme alcohol dehydrogenase (ADH). There are multiple forms of the dimeric ADH molecule, each comprised of different combinations of subunits encoded by separate gene loci. Polymorphisms of ADH do not predict the susceptibility to alcohol-associated liver disease but could explain variations in blood alcohol levels among individuals ingesting the same amount of ethanol.
The acetaldehyde that is generated is subsequently metabolized to acetate, a process that occurs in the mitochondria and is catalyzed by a different enzyme, acetaldehyde dehydrogenase (ALDH). This enzyme, like ADH, has multiple isoforms with differing activities. Genetic variability in ALDH accounts for the well-described flushing reaction among 75 percent of Asians who drink alcohol; this reaction resembles the response to alcohol in patients taking disulfiram (Antabuse).
The flushing reaction in Asians is due to the relative deficiency of ALDH2 isozyme, which results in the accumulation of acetaldehyde. Although acetaldehyde may be a potential accelerant to liver injury, this risk is generally offset by an aversion to further alcohol intake induced by flushing. As an example, the rate of alcoholism among Chinese subjects with this genotype is much lower than in other Chinese subjects; however, a separate reduced genetic risk for alcohol use disorder in this subpopulation cannot be excluded.
The stomach has sufficient ADH activity to metabolize a significant amount of ingested alcohol. A study in 1990 aroused great interest by demonstrating that the metabolism of ingested ethanol in the stomach by gastric ADH was lower in women than men. This was associated with increased levels of ethanol reaching the liver via the portal vein in women. This observation provides a potential explanation for why women seem to have an increased risk of liver injury, compared to men, for a given amount of chronic ethanol consumption. Infection with Helicobacter pylori and gastritis are other factors that can reduce the activity of gastric ADH.
The strongest evidence for alcohol as a cause of liver disease comes from epidemiologic data, not biochemical or clinical studies. As an example, a marked reduction in the number of liver-related deaths was documented in the period after prohibition began in 1916 in the United States. Other data suggest that the risk of alcohol-associated liver disease is related to the amount and duration of alcohol abuse.
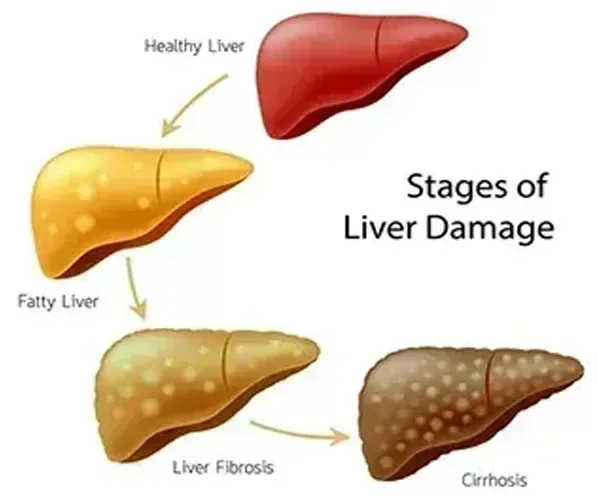
Several factors contribute to the development of alcohol-associated fatty liver including reduced oxidation of hepatic fatty acids and increased lipogenesis. The altered redox state in the liver induced by alcohol impairs beta-oxidation and tricarboxylic acid cycle activity]. Chronic ethanol consumption also increases expression of key lipogenic enzyme regulators, such as sterol regulatory element-binding proteins (SREBPs) and SREBP-1 target genes, such as fatty acid synthase, acetyl-coenzyme A carboxylase, and stearoyl-CoA desaturase.